Stories
-
![]()
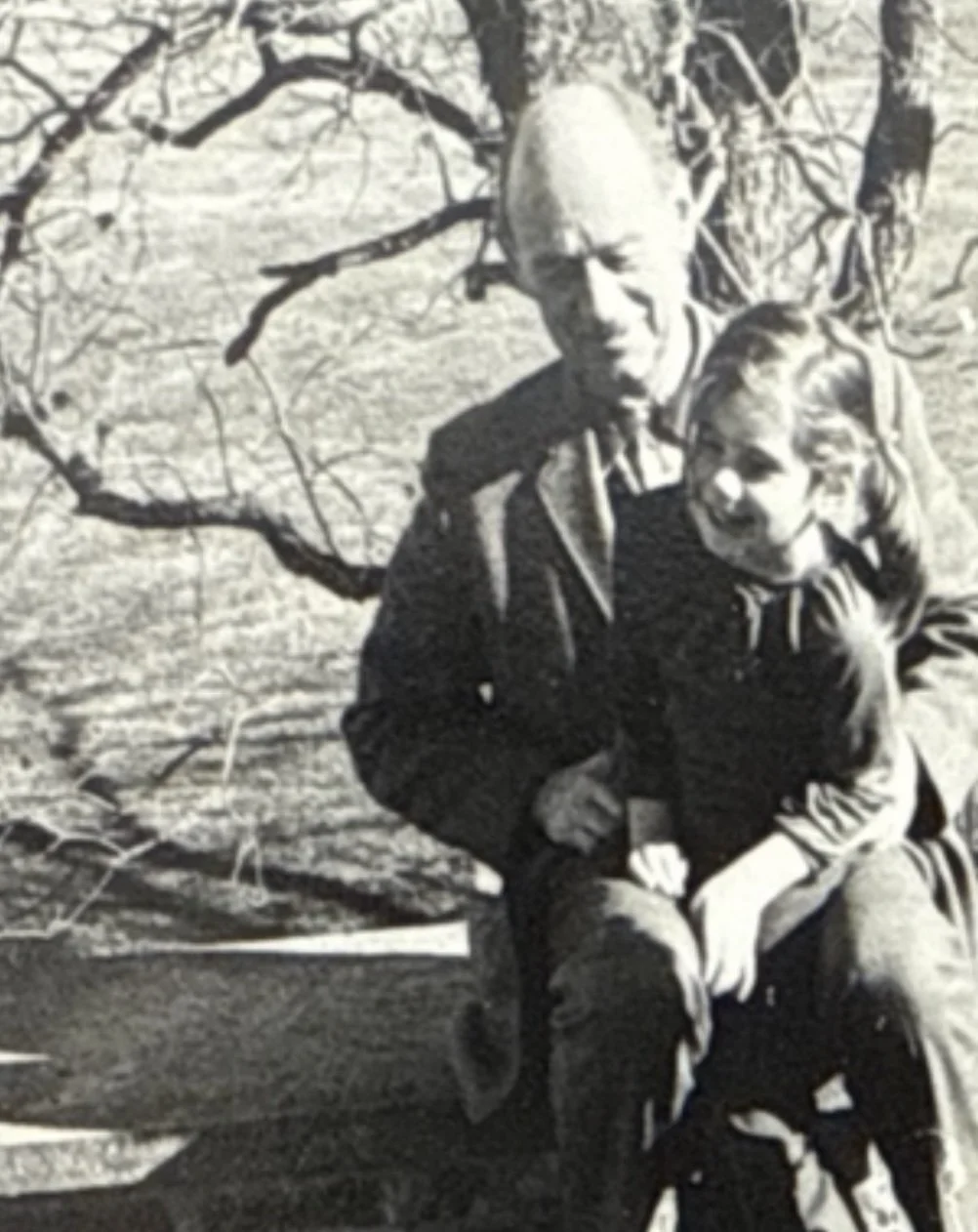
A Lesson in Dignity and End-of-Life Choices
My maternal grandfather taught me valuable lessons about aging with dignity. He was the first to tell me that "pneumonia is an old man's friend"—a belief he held wholeheartedly. He was clear that he wanted no heroic measures at the end of his life.
When he developed pneumonia and ended up in the emergency room struggling to breathe, a well-meaning but uninformed doctor put him on a breathing machine against his wishes. Though the intervention was brief, when my grandfather regained consciousness, he was furious about being "saved." He fell into depression and was prescribed an antidepressant that caused severe constipation—I remember him crying in misery on the toilet.
He did recover and enjoyed acouple more relatively happy years, but he made certain that everyone understood his wishes going forward. When he developed a second bout of pneumonia, this time complicated by heart failure, his passing was quick and comfortable. Although I couldn't make it from Boston in time to say goodbye, it was his time to go—and importantly, on his own terms.
-
![]()
Tillie’s Choice
“Dr. Loengard I think it is time” my patient announced when I returned her call. Tillie had read an article in the New York Times a year earlier about a couple who decided to stop eating and drinking and die together. She was calling to let me know that this was now her plan too. Her time had come she said. Despite being over 90 and enjoying more of what New York City than I did as a young mom – she went to the theater regularly, enjoyed concerts and had many friends in the assisted living where she resided. I told her I would come see her to discuss further. She was one of my patients who was most alive, vital and positive and it seemed impossible that she would want her life to end. I discussed with my colleagues in our morning meeting where each of us would bring clinically or emotionally challenging situations. All agreed with my plan to see her and assess for depression or some other secondary condition that might be influencing her decision to opt out of life. As I entered her apartment, she greeted me with a smile and what always seemed a twinkle in her eyes. As we sat and she humored me by answering the standard depression screening question – finally becoming impatient and exclaiming with a laugh “I laugh at the Daily Show every night, I am not depressed!”. Hard to argue with a 92-year-old who appreciated Jon Stewart. After getting her permission, I spoke with her two daughters, themselves in their late 60’s. They knew of their mother’s plans and despite it making them sad, agreed that she did not seem depressed and her plan to take charge of how she exited this world made perfect sense in the context of her personality and how she had lived her life til now.
She needed a week or so to say her goodbyes and make sure her affairs were complete. Top of her task list was mailing in her ballot for the coming presidential election. When she shared her plans with her adoring long term caregiver Violet, she was so distraught that she could not stay on to help as my patient moved forward with her final plan. Hospice was called and she was enrolled and an out-of-hospital DNR was filled out a posted to her refrigerator. The daughters scrambled and found new people who were willing to help but having people who didn’t know Tillie and her routine proved challenging. After two days of not eating or drinking she was weak and as her aide helped her out of bed, she fell. Unable to stand again and complaining of pain in her leg and hip, 911 was called. Soon after her arrival in the ER, I got a bemused call from the ER physician asking if I knew Tillie and what was going on. Once I acknowledged she was my patient he chuckled and said she had immediately grabbed his tie as he was speaking and looking him sternly in the eye demanded “do not give my IV fluids!”. It turned out her old hip replacement had been jarred out of place and they were able to maneuver it back. A discussion began about how to keep Tillie safe if she went back home. The option of an inpatient hospice bed was brought up and everyone agreed this would be best. Her family could visit and not worry about having to provide medications or being afraid of not having needed support.
I went to see the following Wednesday morning, which happened to be after election day. As I entered her room she was peacefully lying in bed. “Tillie” I whispered. She stirred and half opened her eyes asking me the outcome of the election. When I told her, she closed her eyes again and said “I made the right choice.”
-
![]()
A Bag of Organs
One of the first patients I saw in the house calls program I joined my first year in practice was 88 and lived with his wife of 65 years on the upper west side of Manhattan. He suffered from end-stage heart failure and had declined tremendously in the past year. His mind was still vibrant and his family was close by and supportive. In my first visit we discussed his recent history of multiple hospitalizations due to fluid overload where he would get tuned up and sent home – and then the process would repeat in a matter of days or weeks. As I examined him it was clear he was using all his energy just to breath. He slept in a reclining chair with his head propped at a 45 angle or more. His skin hung from his skeleton and there was swelling in all of his dependent areas, betraying the fact that despite his wife’s good cooking, he was malnourished with low protein levels. When I got to his legs you could push fingers into the swollen skin like risen bread dough, the dents remaining long after the pressure gone. The skin was shiny and red with weeping of fluid. His family was eager to get him to the oldest grandchild’s wedding in 10 days time. We made small changes to his medications and ordered home health to monitor the edema in his legs and check blood pressure as the changes took effect.
The Monday after the wedding I got a call that Mr. Berman was in the ER very short of breath and being admitted to the hospitalist service. At the end of the day I stopped in the hospital before heading home to see my patient and answer any questions. While looking at the patient’s chart I saw the hospitalist who was in charge of his care and inquired about him. “oh he is yours?” he replied “ I am so glad you are here. I have sort of being treating him like a bag of organs!” His reply shocked me. It was a clarifying moment about how medicine should be practiced. Never lose sight of the human being.
As I entered Mr. Berman’s room his eyes brightened and his mouth formed a weak smile. The wedding was wonderful even though he couldn’t dance. He shared how tired he was now though. After talking with his wife and children, it was decided he would go home on hospice the following day and died peacefully on hospice the following week.
-
![]()
Quality of Life? According to Whom?
One of the most striking interactions I had as my father’s caregiver was with the neurologist who followed him after his stroke in November 2019. I had the ‘luck’ of walking into my dad's apartment to find him mid-stroke the Sunday before what was meant to be an 85th birthday party. Lots of people were invited and we had flown in from California. My 11-year-old daughter and I had fetched the cake and were delivering it to his refrigerator for safe keeping. In that moment all plans would change. 911 was called and 10 minutes later he was in a CT scanner which showed a right middle cerebral artery clot. TpA, a couple of nights in the neuro ICU and he was on a regular floor. His life was saved. As his health care proxy, I had made that decision. Once it was done, I wondered frequently if I had done the right thing.
He was left NPO, not allowed to eat, due to his swallow muscles not working well. It happened to be Thanksgiving week and we brought him a chocolate turkey from our family gathering. Unaware or, more likely, not caring about doctor’s orders he consumed the whole thing when I stepped out for thirty minutes. The brown dribble on his gown and multicolored tinfoil crumpled on the table the only remaining evidence. He loved things that tasted good. Beautiful tomatoes, a rack of lamb with mint jelly – and chocolate in any form!
The Neurologist called me the Friday after the holiday to explain that he was recommending a feeding tube. It would be temporary – post-stroke being one of the few times a feeding tube would be recommended in someone 85. As I questioned this approach, the need to keep him NPO and sedation or anesthesia – he immediately jumped in to say “I mean he has a good quality of life!”. We hung up soon after and I found myself saying aloud “Good quality of life according to whom?”. Had anyone asked my dad what he wanted? What was most important? He hated the idea of a tube coming out of his belly, even temporarily. He wanted to eat. To savor what he could. To eat as much chocolate as possible now that gaining weight seemed a good outcome. As the daughter who made the decision to save his life, I had visions of him without food for 3 days and then getting sedation for the procedure, becoming delirious or getting an infection – and never making it home. Paranoid perhaps but bad things happen in hospitals to old people. He and I talked about the possibility of getting pneumonia if he just kept eating, and he reminded me of what my grandfather had said years ago. Pneumonia is an old man’s friend. So we nixed the tube and he went to rehab – and never got pneumonia but ate lots of chocolate ice cream. In the end he got six more months of life and explained to everyone he saw that few people get to know their day of death – the day of his stroke was his.